What is staph?
Staph is found everywhere and can be isolated from air, dust, food, human and animal bodies. Staphylococcus is a member of the skin lice or mucosal mucus.
What is staph?
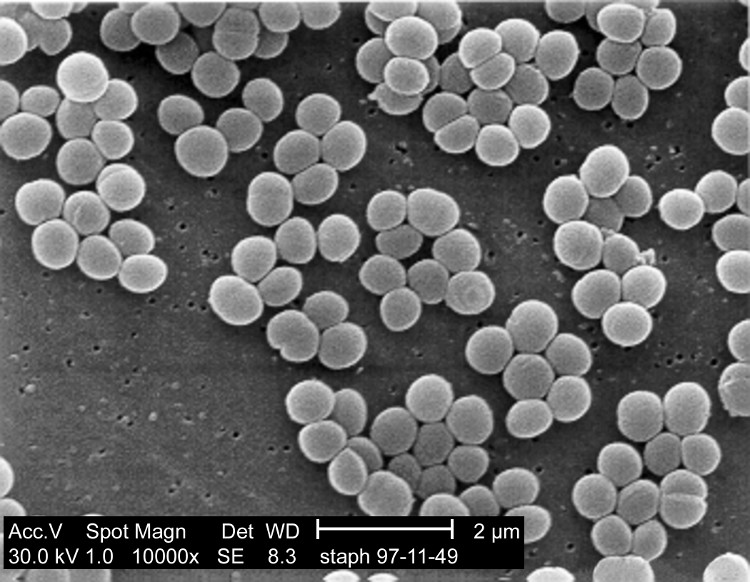
Staphylococci are Gram-positive cocci that do not produce cells about 1 μm in diameter, are not mobile and are arranged in all directions and often form clusters (clusters) that look like bunches of grapes.
It can be said that staph is one of the most famous bacteria: well-known by the famous bacteriologists, the incidence of disease is very high, potentially causing many serious diseases and very antibiotic resistance. strong. The famous microbiologists like Robert Koch (1878) and Louis Pasteur (1880) are very interested in studying staphylococcus at the beginning of the history of microbiology.
On April 9, 1880, Scottish doctor Alexander Ogston presented at the 9th meeting of the German Society of Surgery a scientific report in which he used the concept of staphylococcus and presented relatively well. Enough role of this bacterium in clinical purulent pathology.
Staph.
Classification of staph
In terms of causing disease, staph is divided into two main groups: coagulase and staphylococcus without coagulase.
Staph have coagulase
Thanks to this coagulase, there is blood and bacteria on the culture medium, creating yellow colonies. So this bacterium is also called a golden staph. The important bacteria of this group are:
- Staphylococcus aureus, also known as golden staphylococcus.
- Staphylococcus intermedius.
Staph without coagulase
Because there is no coagulase enzyme, on culture medium there are blood, ivory colonies. Clinically, these bacteria are called white staphylococci. The bacteria of this group may include:
- Staphylococcus epidermidis.
- Staphylococcus saprophyticus.
- Staphylococcus haemolyticus.
- Staphylococcus capitis.
- Staphylococcus simulans.
- Staphylococcus hominis.
- Staphylococcus warneri.
The same 16 strains of staph are not present in humans.
Staph bacteria grow easily on culture media at 37 ° C. The characteristic color of colonies is white like porcelain or ivory white. The hemolytic ability of cultured bacteria provides an important hint of the nature of this bacterium.
In 1926, Julius von Daranyi was the first to discover the correlation between the presence of bacterial plasma coagulase activity and its pathogenicity. However, it was not until 1948 that this discovery was widely accepted.

Staphylococcus aureus staphylococcus aureus culture on soybean jelly trypticase: These strains produce staphyloxanthin yellow pigment.
Characteristics and virulence factors of staph
Clinically, the differentiation of pathogenic and non-pathogenic staphylococcus strains is often based on the presence of Coagulase. This enzyme binds to plasma prothrombin and activates fibrin production from precursor fibrinogen. This enzyme, along with the clumping factor, a bacterial wall enzyme, helps the golden staph create fibrin precipitate on its surface. This property is an extremely important pathogen and the factor also plays an important role in diagnosis.
The golden staph also produces many other virulence factors related to the structure of the bacterial wall.
- Polysaccharide shells: some strains of golden staph can make polysaccharide shells. This shell, along with protein A, protects bacteria against phagocytosis.
- Most strains of staphylococcus aureus have the ability to synthesize a surface protein (protein A) capable of binding to the Fc fragments of immune globulines. Thanks to this unique mounting phenomenon, the number of pieces of FC drops. Because Fc fragments of immune globuline play an important role in opsonin phenomenon: they are receptors for macrophages. The process of attaching above helps golden staph to avoid phagocytosis by macrophages.
In addition, most strains of staphylococcus are capable of producing an intercellular binder. Thanks to this substance, bacteria create a biofilm covering itself and bacteria can grow in mucous membranes.
Extracellular virulence factors of staph
In addition to coagulase and clumping factor, staphylococcus also produces some important enzymes that contribute to the strong virulence of this strain.
- Hyaluronidase : This enzyme has the ability to destroy the basic substance of the organism, allowing bacteria to spread in the organization.
- Hemolysine and leukocidine : destruction of red blood cells (hemolysis) and death of granulocytes and macrophages.
Exfoliatine : enzymes that destroy the epidermis. This enzyme causes skin damage to create blisters. A typical example is Lyell's syndrome due to staphylococci. - Six enterotoxins (Enterotoxine A, B, C, D, E, F) are stable to heat . These enterotoxins play an important role in food poisoning.
- Toxins cause poisoning shock syndrome : the cause of toxic shock syndrome, a severe shock syndrome.
- Most strains of staphylococcus are produced by penicillinase (beta-lactamase) . This enzyme destroys the beta-lactam ring, the basic structure of antibiotics such as penicilline G, Ampicilline and Ureidopenicilline, making these antibiotics ineffective.
The role of clinical staphylococcus aureus
1. Disease caused by invasive staphylococcus
Localized infections in the skin and mucous membranes: skin infections and dependent parts (mainly the hairs and sweat glands) forming a classic abscess of staph. Staphylococci have the ability to create fibrin thus creating a fibrin wall covering the abscess. These infections may be as small as a pin tip (hair folliculitis) or the size of an apple in an abscess. Areas of skin covered with dense hair, staph often cause bumps. Local lesions can be mild but it is also a risk of spreading bacteria to more distant organs. Pus of abscesses due to staphylococcus aureus is usually yellow, dense and non-foul.
Infections of deep organs: infection of internal organs can be caused by endogenous: from an infection of the peripheral infection, bacteria along the blood and lymph pathways to other organs. Infection can also be caused by exogenous causes: bacteria travel from the environment into the body through a skin tear after an injury or during surgery. Typical diseases in this group may include: bone marrow osteomyelitis, sepsis, sinus vein thrombophlebitis, endocarditis, pus meningitis .
2. The medium
- Blanching dermatitis (neonatal flaking, staph skin syndrome) is common in infants and young children. The causative agent is the staphylococcus strains producing Exofoliatine. Immediately after the symptoms of fever and redness of the skin, the disease is characterized by signs of peeling of the epidermis while forming a large blister. The disease is usually benign. Although large blisters appear on the skin, they rarely lead to disorders of water and electrolytes. New skin is formed quite quickly. Similar to this pathology is Lyell Syndrome due to Staphylococcus and Staph infection.
- Toxic shock syndrome: common in young women during menstrual periods with strong absorbent bandages. Because of this good absorbency, the tape has a longer use time. Some of these absorbent cottons are able to bind to magnesium ions thus reducing the amount of this ion in the vagina. About 20% of women carry staphylococci in the vagina. Because magnesium ions decrease, this bacteria enhances the production of shocking foreign toxins. Clinical conditions of toxic shock syndrome include sudden high fever, fatigue, watery diarrhea, headache, muscle pain, skin rash and one or more signs of shock. This syndrome has a relatively high mortality rate.
- Thukydides syndrome: is a special form of toxic shock syndrome. This syndrome can occur in adolescents of both sexes, often due to superinfection of staphylococcus after flu. The mortality rate of this syndrome is very high (over 50%). Respiratory and gastrointestinal manifestations are very similar to the plague described by Thurykodides in Athens and 430 BC.
3. Disease caused by toxins
- Food poisoning is the most typical disease caused by intestinal toxins that are stable to the heat of staph. After eating cold foods or even staph contaminated foods have been cooked. Can be divided into two forms:
- Gastroenteritis: the cause of ingestion of staphylococcal food. The disease usually occurs in a short time with symptoms of severe vomiting, watery diarrhea, no fever. The disease usually heals quickly and does not require antibiotic treatment.
- Small-colon intestinal inflammation: caused by food contaminated with large amounts of staph bacteria (> 105 bacteria / g food) or by bacteria growing in the intestine (up to 2-30% of carriers) bacteria in the intestine). Gastrointestinal symptoms such as abdominal pain, vomiting, prolonged diarrhea and need for antibiotic treatment.
- Food poisoning caused by staphylococcus aureus in Vietnam is common in weddings. Because it has to prepare for many diners (about 200 people on average), food needs to be cooked first and left overnight. Staph infection from the environment or from the processor will proliferate very quickly in foods with a suitable nutrient content (most commonly eggs, cold meats), and produce intestinal toxins. This toxin is very resistant to heat, so it is impossible to pre-boil it before boiling it. When you eat food with intestinal toxin, after 30 minutes to 1 hour are symptoms of vomiting, diarrhea has occurred.
Prevention of staph
Staphylococcus usually tolerate environmental changes such as drought, sunshine, temperature, pH and salinity changes. Medical personnel are those with extremely high rates of carrying bacteria. Measures such as wearing hats or headscarves, veils or masks and frequent hand washing are the best methods of preventing transmission of bacteria in hospitals especially in recovery units. These measures also apply to people working in collective kitchens or food processing workshops.
The percentage of people carrying staphylococcus aureus in the skin or mucosa ranges from 10 to 90%. Common areas of staphylococcus aureus are vestibular, hair, armpit and anal folds. This is a source of cross-contamination in resuscitation units, especially in immunocompromised patients such as diabetes, AIDS or cirrhosis. The dangerous bacteria in these areas are golden staphylococcus resistant to methicillin.
Staph without coagulase
Staph without coagulase is part of the normal bacterial flora of the skin and mucosa. The most important representative of this group is Staph. epidermidis.
For a very long time, microbiologists considered this bacterium to be non-pathogenic. But today it is well known that staph do not have coagulase, especially Staph. epidermidis is a common cause of orthopedic surgery and is also the cause of hospital infections. These bacteria are capable of forming a mucous membrane and under this mucous membrane, the bacteria grow into small colonies that attach to plastic catheters. This mucus also protects bacteria from being attacked by immune body cells and is not affected by antibiotics.
Staphylococcus saprophyticus is the common cause of urinary infections in young women because this bacterium has the ability to adhere to urinary epithelial cells and produce urease enzymes.
Treatment of infections caused by staphylococci without coagulase is often difficult because the bacteria are often resistant to antibiotics. Another reason is that it is difficult to determine exactly which agents in this group of bacteria cause specific treatment because they are usually present on the skin and mucosa.
- Signs of staph infection anyone should not be ignored
- New staph can cause death in 72 hours
- Birth control pills increase staph infection
- How does golden staph bacteria enter through dangerous food?
- Video: Risks to the body when stabbed or thorny
- Golden bridge - 'defending champion' antibiotic resistance
- Computers help chemists fight off acute infections
- The virus invades the beaches
- Potential risk from carrying food
- Antibiotics from dirt
- The most toxic and strange forms of bacteria on the planet
- Find out what new antibiotics help overcome drug resistance
 Why do potatoes have eyes?
Why do potatoes have eyes? 'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet
'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet Tomatoes were once considered 'poisonous' for 200 years
Tomatoes were once considered 'poisonous' for 200 years Detecting microscopic parasites on human face
Detecting microscopic parasites on human face