Ancient bacteria causing leprosy are mutating
We will need to combine 3 drugs, even more to combat this disease.
According to a new study in the journal Nature Communications: Mycobacterium leprae - causing leprosy - is getting stronger and extremely resistant. Their genome is mutating crazily in agony to maintain the ability to kill people over time.
This alarming situation was discovered by scientists from the genome survey of 154 M. leprae species, collected from 25 countries around the world. Its results provide a rare genetic view of this ancient, mysterious and dangerous bacterium.
Appearing and existing from the Iron Age (1200-600 BC), M. leprae is still causing 200,000 new cases of leprosy each year worldwide, concentrated in South America, Africa. , South and Southeast Asia.
Ancient bacteria that cause leprosy are mutating "crazy" resistant to antibiotics.
The research is under the cooperation of scientists from many countries, led by microbiologist Stewart Cole of Lausanne Polytechnic University, Switzerland. They note that the super-mutant state of M. leprae "may facilitate the emergence of resistance."
Super-mutations make the bacteria stronger, seemingly in its own agony. Because M. leprae has a short genome, super mutants "can cause damage and lead to their deaths" . Basically, this high rate of mutation can damage the genes needed for the life of bacteria.
A global look at the genome of M. leprae strains is a rare opportunity, despite the long history of these bacteria with humans. M. leprae may have appeared to cause leprosy from the Iron Age, 1200-600 BC.
In 1873, Dr. Gerhard Henrik Armauer Hansen was the first to correctly identify this. He reported that when water is dripped into cells flaking from the leprosy body, a number of "rod-shaped organisms" fill out.
These rod-shaped creatures are M. leprae. And Dr. Hansen's observation is the first time in the history of bacterial confirmation of a chronic disease. Hansen's discovery also made leprosy named after himself, Hansen's disease .

These rod-shaped creatures are M. leprae.
A complex epidemic
Even so, until more than a century later, human knowledge of leprosy is still relatively small. M. leprae is difficult to study, due to its unique biological properties. M. leprae develops slowly, survives inside cells, and spreads quietly.
Therefore, scientists have yet to find a way to cultivate this strain of bacteria in a laboratory environment. How exactly does M. leprae cause illness? Why is it killed by some antibiotics? And its path of infection is still the question to be answered.
Meanwhile, M. leprae is still a threat to public health in South America, Africa, South Asia, Southeast Asia, and Micronesia of Australia. This bacterium is causing about 200,000 new leprosy cases each year.
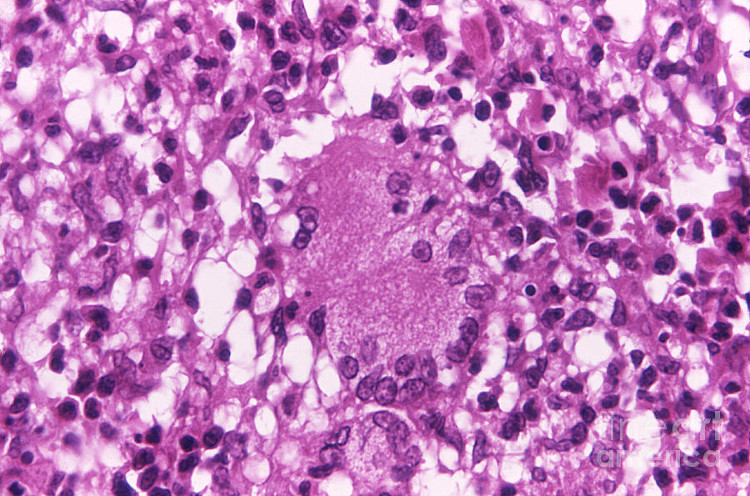
When M. leprae infects humans, researchers know that it usually resides in peripheral neurons. Some evidence suggests that M. leprae reprograms cells to a "stem cell-like" state.
Infection leads to inflammation, granuloma, and systemic spread of bacteria in the patient's body. Finally, patients with M. leprae infection will experience loss of sensation, atrophy and gradual loss of fingers, toes and limbs. Untreated, leprosy can be fatal.
Until now, researchers are still unsure about what mechanism the M. leprae bacteria causes and how it can appear in the victim's body. Direct human-to-human transmission is the highest possibility.
But there are also some experts suggesting M. leprae spread to humans from insects and animals. Previously, this bacterium was found in mice, apricot animals, red squirrels, and some non-human primates.
In the past, the only way for scientists to have enough M. leprae for genetic studies was to infect it in mice and animals in the lab. However, they will still have to wait a year.
M. leprae takes 14 days to grow through a generation. In comparison, E. coli can do this within 20 minutes. The slow development, along with the intracellular residence of M. leprae, makes extracting it from human tissue extremely difficult.
But in this new study, Cole and his colleagues solved the problem. They devised an optimization method to isolate M. leprae. The trick is to punch a hole into human cells, degrade our DNA. Later, Cole tries to break the bacteria and collect as much of their DNA as possible.
In this way, M. leprae's DNA will be collected with little and no human's DNA.

Patients with M. leprae infection will lose their sensation and gradually lose their fingers and toes.
Super mutant
Cole's team analyzed the genome of M. leprae from 147 human leprosy samples, 6 red squirrels and an apricot creature. These samples are selected from all over the world. They are all taken from organisms that carry natural infections.
They looked at how M. leprae strains are related to each other, the way they appear and the mutations associated with drug resistance.
From their analysis, the researchers found that the oldest M. leprae strains came from East Asia. This is consistent with previous studies, showing that leprosy originated in Eurasia and spreads along human migration routes into Africa and the Americas.
However, researchers have shown 8 strains of M. leprae super mutants. These strains of bacteria have a lot of mutations in the entire genome.
They mutate frantically enough to break a normal gene that will allow bacteria to test and fix DNA. This explains why the mutations of these M. leprae strains can explode.
The team also noted the development of antibiotic resistance, especially in some super mutant bacteria. Since the 1980s, to treat leprosy, we have had to combine two to three types of antibiotics, typically rifampicin, dapsone and clofazimine.
Even so, doctors do not know how clofazimine killed M. leprae. Before 1980, they sometimes only needed to prescribe a single antibiotic to treat the disease.

Areas where different M. lepae strains are collected.
For some strains of M. leprae that are resistant to three or more antibiotics, the researchers looked at the patient's medical records, thereby isolating these strains.
Their research shows that, in some cases, multi-drug resistant M. leprae strains have been transmitted from patient to patient for decades. They develop resistance to each new antibiotic that humans tested.
"Drug resistance is very alarming during leprosy control ," scientists wrote in the survey results. "Their new research has dug up completely new mutations that can make it difficult for us to make a difference. drug resistant bacteria, in ways never observed ".
"Our findings on these mutations . encourage further trials to determine their true role and contribution to antibiotic resistance [M. leprae]." , the study concluded.
- Find out the oldest infectious bacteria of humanity
- Decode the disappearance of leprosy in Europe
- Rapid test equipment for leprosy
- The first person to find a leprosy medication was a female scientist
- WHO warns that leprosy is spreading rapidly in India
- How dangerous is the caterpillar poisoning?
- The oldest evidence of leprosy in India
- Bacteria that live over 50,000 years in caves in Mexico
- Bacteria more than three billion years old hide in the cave
- Bacteria protect ancient paintings from bacteria that eat pigments
- H. pylori ulcer bacteria can prevent diarrhea
- Treat acne with a virus
 Why do potatoes have eyes?
Why do potatoes have eyes? 'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet
'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet Tomatoes were once considered 'poisonous' for 200 years
Tomatoes were once considered 'poisonous' for 200 years Detecting microscopic parasites on human face
Detecting microscopic parasites on human face