Hydrocephalus in children: Causes, identification signs and prevention
Hydrocephalus is not a separate disease but rather a consequence of a group of different diseases that share a common feature of impaired circulation or absorption of cerebrospinal fluid.
1. Physiology
Cerebrospinal fluid is primarily formed in the ventricular system due to discharge of mesenteric plexus . This tangle is located in the two ventricular ventricles, the ventricular ventricular and the ventricular four but mainly in the two side ventricles.
The total amount of cerebrospinal fluid is 50ml in children and about 150ml in adults. Cerebrospinal fluid is considered ultrafiltration of plasma. The cerebrospinal fluid travels from the two lateral ventricles through the Monro hole to the ventricular third and then flows through a narrow structure called the Sylvius canal into the ventricular four. In children, this channel is about 3 mm long and 2mm in diameter. From the fourth ventricle, cerebrospinal fluid follows two lateral holes (Luschka hole) and a middle hole (Magendie hole) to fill the reservoir in the brain background. Hydrocephalus as a result of blockage of the ventricular holes and channels of the ventricles is called obstructive hydrocephalus or unresponsive hydrocephalus.
A very small part of the cerebrospinal fluid is absorbed by the lymphatic system that flows to the sinuses around the nose, another part is absorbed along the nerves and by the vascular plexus itself. For some reason, the subarachnoid chambers are clogged or the spider nodes (arachnoid granulations) function impairment also causes hydrocephalus. Hydrocephalus in this case is called an unobstructed hydrocephalus or a hydrocephalus.
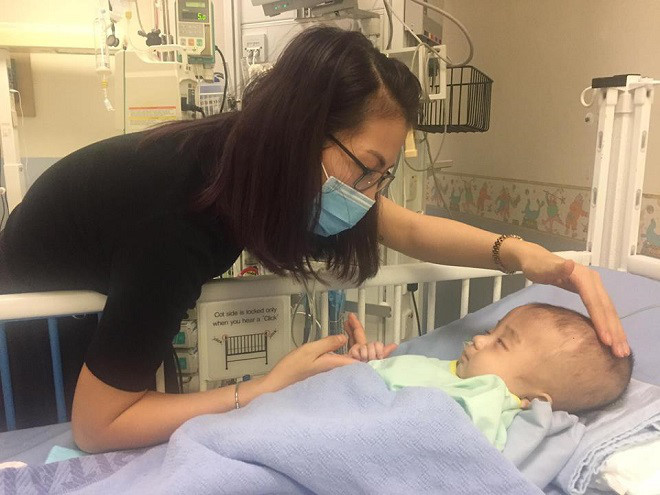
A baby with hydrocephalus.
2. Pathophysiology and causes
- Obstructive hydrocephalus or unresponsive hydrocephalus usually occur primarily in children due to abnormalities of channel Sylvius or due to quadriplegic damage. Channel structure abnormalities Sylvius often cause narrowing of the medullary fluid circulation. Due to pus meningitis or cerebral hemorrhage in the neonatal period, the myeloid cells lining the ventricles peel off, causing spider cells to be proliferated to cause narrowing of the channel. Infection in the fetal stage, commonly known as TORCH (Toxoplasmosis, Rubella, Cytomegalovirus, Hepatitis) are also causes of hydrocephalus. Brain tumors, especially posterior pituitary tumors, interfere with cerebrospinal fluid circulation and cause hydrocephalus very quickly with very severe signs of intracranial hypertension in older children. Birth defects that cause hydrocephalus may include Chiari deformities, Dandy - Walker syndrome .
- Unobstructed hydrocephalus or hydrocephalus is often the result of intracranial hemorrhage, often in preterm neonates or infants with vitamin K deficiency. Pneumococcal meningitis or meningitis due to The tuberculosis causing secretions adhered to spider nodes (arachnoid granulations) also impaired the function of these absorption nodes. Complications of meningitis of acute leukemia are also possible causes of hydrocephalus.
3. Clinical manifestations
The clinical manifestations of hydrocephalus vary widely from case to case and depend on many factors such as:
- Age of disease.
- The nature of the injury causes blockage of cerebrospinal fluid circulation.
- Time sick.
- Speed of increased intracranial pressure.
In young children because the skull joints are not closed yet, the most visible symptom is the size of the head that grows abnormally quickly. In addition, the frontal font is also enlarged and stretched, the scalp blood vessels are also enlarged more than usual. Young forehead is very wide. The naked eye in a downward-looking posture creates a sign of the setting sun.
In older children , when the skull joints are partially closed, the big head signal is more unrecognizable. Symptoms suggest easy irritation, irritability, fatigue, loss of appetite, and vomiting. Highlights in this group of children are symptoms of headache. Other signs can be seen as thorny edema, signs of damage to the tower bundle . Two groups of common birth defects causing hydrocephalus are Chiari deformities and Dandy - Walker syndrome.

Clinical manifestations of altered hydrocephalus vary greatly from case to case.
Chiari has two subgroups:
- Type I Chiari : symptoms often manifest in older children and adults, often rarely with hydrocephalus. Patients often suffer from recurrent headaches, neck pain, urination, and worsening lower extremities. This abnormality is often characterized by falling cerebellum almonds into the medullary canal. The cause of this condition is unknown but may be due to blockage of the lower part of the ventricle 4 during fetal development.
- Chiari type II: characterized by hydrocephalus developing gradually and meningeal hernia. This damage is due to abnormalities of the posterior brain, which may be due to normal brain angulation during embryogenesis, causing the ventricular 4 to be prolonged. Consequently, the twisted brain stem makes the lobe worms, brain bridges, and marrow onions go into the medullary canal. Approximately 10% of children with deformity of type II malaria appear right from the newborn period such as wheezing, weak crying, apnea. These symptoms are reduced if surgery to drain the cerebrospinal fluid early.
Dandy - Walker syndrome is an abnormality of the ventricular 4. In this malformation, the ventricular quadrangle dilates into a follicular form because the ventricular ceiling is abnormally developed during embryo formation. About 90% of Dandy - Walker malformed patients exhibit hydrocephalus. A large number of patients also have accompanying abnormalities such as aplasia of the cerebellar worms and the corpus luteum. Children often have a very large head size and a prominent occipital area. Children often exhibit loss of movement, mental retardation, seizures .
4. Diagnosis
- Balanced disorders and walking (the earliest symptoms) : The short and the legs are wide apart. In severe cases, it is impossible to walk without help .
- Sphincter disorder : uncontrolled urination (late stage).
- Dementia - Forehead syndrome : Slow mental development, attention disorders, memory disorders. In some cases, symptoms similar to Alzheimer's disease, surgery does not produce good results
These symptoms are not very specific for hydrocephalus: difficult clinical diagnosis, laboratory testing gives more accurate results.

Most cases of hydrocephalus require surgical treatment aimed at draining cerebrospinal fluid from the brain.
5. Additional testing
- Brain CT scan (without contrast injection) shows that the 4 ventricular dilatation does not expand the cortical grooves (helps distinguish between hydrocephalus and brain atrophy).
- Brain magnetic resonance imaging (MRI) is the selected test. It helps to show evidence of ventricular dilatation and abnormalities around the ventricles.
- Suppressing cerebrospinal fluid sometimes helps to temporarily improve symptoms (especially standing symptoms). Analysis of normal cerebrospinal fluid.
6. Treatment
Treatment depends on the cause of the disease.
- Medical treatment : taking drugs such as acetazolamide and furosemide may temporarily reduce the production of cerebrospinal fluid. However, the long-term effects of these drugs are very limited. In addition, children with hydrocephalus may also have other symptoms such as epilepsy, medical treatment is also to control these pathological manifestations.
- Most cases of hydrocephalus require surgical treatment aimed at draining cerebrospinal fluid from the brain. The most commonly used surgery is to place the ventricular drainage - abdomen. This surgery takes a soft tube under the skin, a tube in the ventricle, the other end in the peritoneal cavity of the abdomen. Cerebrospinal fluid in the ventricular duct drains into the peritoneal cavity. Here the fluid is absorbed and returned to circulation.
- A complication of drainage is infection, most commonly a staphylococcus (staphylococus epidermidis). However, if surgery is done carefully, the rate of infection can be lowered to 5%. Currently in advanced perinatal centers one can conduct this drainage surgery as soon as the child is still in the womb. However, the results of the above saved cases are not very satisfactory. The reason is that when a child exhibits a hydrocephalus in the fetus that requires surgery, the cause is usually the syndrome of many different malformations associated with one patient.
- Hydrocephalus in children: Treatable if taking advantage of
- Signs help us recognize lung cancer
- Young anemia and identification signs
- How to manage and prevent eye injury in children
- New Identification Technology
- Signs of identification and prevention of diphtheria
- How to recognize early thunderstorms, cyclones, hail
- Signs to recognize whooping cough parents need to know
- Early signs of lung cancer identification
- Signs that the child has been abused parents need to know
- 9 signs of twins identification
- 10 signs of cancer are growing in the body, everyone must be satisfied
 Green tea cleans teeth better than mouthwash?
Green tea cleans teeth better than mouthwash? Death kiss: This is why you should not let anyone kiss your baby's lips
Death kiss: This is why you should not let anyone kiss your baby's lips What is salmonellosis?
What is salmonellosis? Caution should be exercised when using aloe vera through eating and drinking
Caution should be exercised when using aloe vera through eating and drinking