Simple change turns cells into embryonic stem cells
Finally, Biologists have lost patience with cloning failures. This achievement can be a common buzz for the field of therapy cloning.
Studies published last week by three different research groups showed that it is possible to reprogram normal skin cells into an embryonic stem cell in mice . The race now turns to this surprisingly simple technique for human cells. If the researchers succeed, the creation of cells of the nature of stem cells, and the genetic material that matches the patient will become quite easy. There are some limitations on the usefulness and safety of these results in therapeutic applications in the near future, but in laboratories these results quickly bring about an exciting atmosphere.
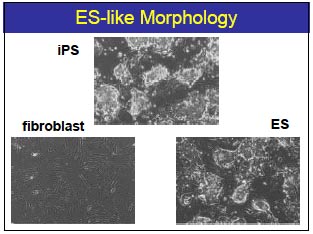
Compare images of iPS, fibrous cells and embryonic stem cells.
"It will change a lot about our views , " said Alan Trouson of Monash University in Australia. Trouson is not the one who made these results directly but claims that he will start using the technique right away 'tomorrow'. "I can think of dozens of experiments now and all are good experiments."
In theory, embryonic stem cells can proliferate indefinitely and can become any type of cell in the body. However, so far the only way to obtain embryonic stem cells is to destroy the embryo and to obtain a suitable genetic embryonic stem cell for the patient, in principle, to clone the patient. All of these techniques give rise to ethical problems that are difficult to solve. Besides the ethical difficulties, cloning is not easy. This process involves collecting unfertilized eggs, replacing the genetic material of the eggs with genetic material from the patient's cells and forcing the cells to divide to create embryos, then collecting stem cells. ingot. These barriers have now been removed.
"No eggs or embryos are needed. And I have never worked with them." Shinya Yamanaka at Kyoto University, who pioneered this new technique, said.
Last year Yamanaka was the first to use a technique in which people use mouse fibroblasts, a common type of cell that is easily taken from the skin instead of eggs. Four genes coding for four proteins of transcription factors are transferred into cells by retroviruses. These proteins activate the expression of other genes, making cells become universal, meaning they can become any cell in the body. Yamanaka calls them induced pluripotent stem cells (iPS cells)."It's as easy as it is. There's no miracle here." Yamanaka said.
This result has brought many surprises and doubts. Four factors seem too little. And although these cells have the characteristics of stem cells such as colonies, continuous proliferation and the ability to develop into cancer cells, called teratoma . they still lack some properties. other importance. Incorporating iPSs into developing mouse embryos does not create 'mosaic mice', ie mice that carry a mixture of DNA from both the original embryo and iPS cells throughout the body."I was not very comfortable with the word" universal "last year, Hans Scholer, a stem cell specialist at Max Planc Institute.
Last week, Yamanaka launched a second generation of iPS, meeting all the above criteria. In addition, another research group led by Rudolf Jaenisch of the Whitehead Institute, in collaboration with Konrad Hochedlinger at the Harvard Stem Cell Institute and Kathrin Plath at UCLA, also obtained similar results with the four transcription factors.
"We feel relieved because some people have questioned their results, especially after the Hwangate scandal , " Yamanaka said. Scholer also agreed: "Now we can confidently say that this is something worth developing."
Improving the results of the previous year is quite simple . The four transcription factors that Yamanaka used did not re-establish the genome consistently and effectively, so less than 0.1% of the millions of cells were reprogrammed. The difficulty here is to separate successfully reprogrammed cells from the remaining cells. Researchers often do this by installing an antibiotic resistance gene. This gene is expressed only when the transcription factor is expressed. They then put these cells into an antibiotic-containing medium. Antibiotics will kill cells that are not reprogrammed. The protein that Yamanaka used last year was not very good at identifying reprogrammed cells. This time all three groups used two other types of protein markers, Nanog and Oct4, to achieve the desired effect. All three groups can produce mosaic mice with iPS cells separated in this way; and these mice transmitted the iPS DNA to their children.
Jaenisch also succeeded in using a special embryo to create pregnancies with all cells derived from iPS."Only the best embryonic stem cells can do this," he said.
"It's unbelievable, it's simply amazing," Scholer said when he heard Jaenisch's report at a seminar on May 31 in Bavaria. "For me this is like Dolly. It's really big."

The creation of mosaic mice demonstrates that iPS cells are not unlike other embryonic stem cells
This method proved very attractive. While cloning is limited in the number of eggs and complicated techniques, it takes up to six months to become proficient, Yamanaka's method can use the simplest cells and can be done using techniques. Simple laboratory techniques.
However, the application of this method to people has not been successful."We are working very hard - day and night. Maybe we need more transcription factors." Yamanaka confided.
If successful, researchers can create iPS from patients with Parkinson's disease, diabetes and monitor molecular changes in these cells as they develop. The "Petri-disc disease" method will give scientists an opportunity to know how environmental factors affect the process of disease formation and can test the ability of different drugs in inhibition of disease development.
However, iPS cells are not without defect. It is not possible to use them safely to create genetically suitable cells for tissue transplantation, for example, to treat spinal cord injuries. Yamanaka discovered that one of the transcription factors seems to play a role in creating cancer in 20% of the mosaic mice he created. He thought that this could be solved, but the retroviruses themselves could also cause mutations and cancer."This is very dangerous. We will never transplant these cells for patients," Jaenisch said. In his view, embryonic stem cell research will still require cloning.
Following this momentum, there will be good news soon."I'm not sure if it will be us, or Jaenisch, or another person, but I expect a great success on people next year, " Yamanaka said.
References:
1. Okita, K., Ichisaka, T. & Yamanaka, S. Nature doi: 10.1038 / nature05934 (2007).
2. Wernig, M. et al. Nature doi: 10.1038 / nature05944 (2007).
3. Maherali, N. et al. Cell Stem Cell doi: 10.1016 / j.stem.2007.05.014 (2007).
4. Takahashi, K. & Yamanaka, S. Cell 126, 663–676 (2006).
Nguyen Ngoc Luong
- 10 ways stem cells promote medical development
- The man creates embryonic stem cells
- Successfully created kidney cells from stem cells
- What are stem cells? How advanced is medicine in this area?
- Blindness with human embryonic stem cells
- Going to test human embryonic stem cell therapy
- Mapping the first gene of 5hmC molecule in human embryonic stem cells
- For the first time successfully created stem cells from human skin
- New method to create human stem cells
- Treatment of deafness by stem cell method
- Improved mature cells mature
- Detecting the mechanism of change of embryonic cells
 Why do potatoes have eyes?
Why do potatoes have eyes? 'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet
'Tragedy' the world's largest carnivorous life: Death becomes ... public toilet Tomatoes were once considered 'poisonous' for 200 years
Tomatoes were once considered 'poisonous' for 200 years Detecting microscopic parasites on human face
Detecting microscopic parasites on human face