Causes and risk factors of rheumatoid arthritis (Part 1)
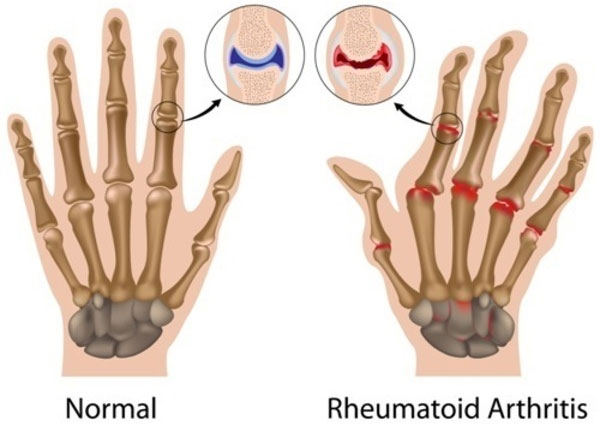
People often think that rheumatoid arthritis and osteoarthritis are the same disease. However, these are two completely different diseases.
Osteoarthritis is caused by long-term damage to the joints, while rheumatoid arthritis is a more complex and confusing disease, when the body's immune system attacks its own cells and tissues, including both joints, skin and organs.
Like other autoimmune disorders such as lupus and psoriasis, the cause of rheumatoid arthritis is still not well understood. What we already know is that some factors - including smoking and obesity - can not only increase the risk of disease but also experience worse symptoms.
Common causes
Rheumatoid arthritis occurs when the body's immune system "fails". Often, the body produces defense proteins (called antibodies ) that are "programmed" to find and attack the causative agent (called an antigen ).
For unknown reasons, the body will sometimes produce antibodies that confuse normal cells into harmful cells. Depending on the type of disease, autoimmune disease can occur throughout the body (affects many organs) or is determined (affecting 1 or more organ systems).
In rheumatoid arthritis, part of the "programmed" immune system falsely blocks antibodies that target joints. The "culprit" of this abnormality is thought to be due to variants of the human leukocyte antigen (HLA) system, which controls the immune response.
The genes are able to play a role in abnormalities including:
-
STAT4 : A gene plays a role in regulating and activating immune responses.
-
TRAF1 and C5 : 2 genes are linked to chronic inflammation.
-
PTPN22 : A gene involved in both formation and progression of rheumatoid arthritis.
It is possible that only a combination of gene variants and / or gene mutations are sufficient to activate the disease. But not everyone who carries this gene will have rheumatoid arthritis and not all people with rheumatoid arthritis have these genes.
This suggests that · there is a possibility that other factors may trigger an autoimmune reaction, especially if you are at risk of genital rheumatoid arthritis. One theory is that certain bacteria or viruses may inadvertently "confuse" the immune system. Four infections can trigger rheumatoid arthritis in some people, including:
-
Epstein-Barr Virus (EBV)
-
Escherichia coli (E. coli)
-
Hepatitis C virus (HCV)
-
Mycobacterium
Scientists believe there may be cross-reactivity between these antigens and some normal cells of the body. Thus, antibodies produced in response to EBV may consider EBV and normal cells the same. Then, even if EBV infection is resolved, the body will remain in a high alert state and be ready to react to any suspected EBV cells.
There may also be other factors that cause the immune system to malfunction. With some factors, we can change them, but for others it doesn't.
Risk factors cannot be changed
Rheumatoid arthritis affects certain groups more than others. The three irreversible factors often associated with this disease are age, gender and family history of rheumatoid arthritis.
Age
While rheumatoid arthritis can attack at any age, the onset of symptoms usually begins between the ages of 40 and 60. Moreover, the risk increases as age increases.
Sex
Women are three times more likely to develop rheumatoid arthritis than men. Although the explanation for this difference is unclear, hormones in women are thought to play a role in disease formation.
This is partly demonstrated by a study that has shown that the disease usually appears after a major hormone change. This sometimes occurs immediately after pregnancy or parallel to the early period of menopause. The cause is thought to be due to hormones Estrogen, and especially the decline of this hormone.
On the other hand, using estrogen replacement therapy may provide a protective benefit for older women, who are at high risk.
Young women who are using birth control pills may also have such benefits. According to researchers at Stockholm's Karolinska Institute, women who have used estrogen-containing birth control pills for more than 7 years have reduced their risk of the most common rheumatoid arthritis compared to women who have never been use birth control pills.
Genetic
People with parents or siblings with rheumatoid arthritis are 3 times more likely to develop the disease than the average person. Or even having close relatives who are sick will double the risk of disease. These numbers help illustrate the central role of genetics in the development of autoimmune disorders.
According to a 2016 study published in the journal Lancet, genetic factors account for about 40% to 65% in all confirmed cases. While precise genetic mutations have not been identified, people with autoimmune diseases are thought to have one or more mutations that change the way the immune system recognizes and targets pathogens.
One of the main doubts is the HLA-DR4 gene, one of the gene variants associated with other autoimmune diseases such as lupus, rheumatoid arthritis or autoimmune hepatitis. Research from the University of Michigan has also concluded that people with another HLA-related genetic marker are five times more likely to develop rheumatoid arthritis than those who do not carry this genetic marker.
(Continue.)
- Causes and risk factors for rheumatoid arthritis (Part 2)
- Many people with rheumatoid arthritis do not know
- Eating fish reduces the risk of rheumatoid arthritis
- Rheumatoid arthritis because of eating a lot of meat
- Rheumatoid arthritis makes it difficult for women to become pregnant
- High cholesterol, a warning sign of rheumatoid arthritis
- No association between rheumatic inflammation and air pollution?
- Everything you know about Vitamin D has never been wrong
- Three new drugs that treat rheumatoid arthritis effectively
- Regular brushing reduces the risk of arthritis
- 5 types of dangerous diseases can be detected by eye examination
- Osteoarthritis is common in pregnant and postpartum women
 Chinese doctors have created medical masks that cover only the nose for convenience of eating and drinking
Chinese doctors have created medical masks that cover only the nose for convenience of eating and drinking Scientists have found a way to help you regrow new teeth after only 2 months
Scientists have found a way to help you regrow new teeth after only 2 months Do non-stick pans cause cancer? What alternatives are there?
Do non-stick pans cause cancer? What alternatives are there? Blisters around the body: Causes, symptoms and treatment
Blisters around the body: Causes, symptoms and treatment