Latest model of Alzheimer's causes
Recently, a team of researchers at Yale University discovered a protein that plays a key role in the development of Alzheimer's disease (AD). Research shows that when the activity of this protein is prevented by an existing drug, experimental mice implanted with AD brain models showed memory recovery.
Alzheimer's (AD) is a disease of modern life. 10% of people over the age of 80 suffer from this disease and the number of patients worldwide is expected to increase to about 100 million by 2050. AD is detected as a combination of many special symptoms from In the first year of the 20th century, however, this disease has appeared for a long time in human history. In the past, AD was not considered a big problem for daily life. Human life is much shorter now and people will die before Alzheimer's disease. For this reason, we do not have effective protection mechanisms for the evolution of AD whether through natural evolution or through the development of medicine and biology.
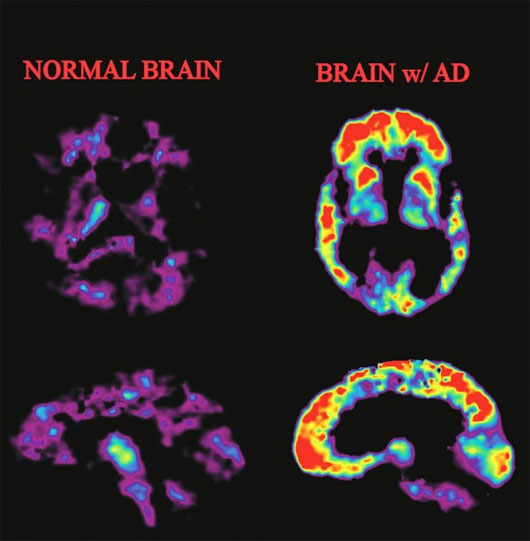
The brain of a normal person (left) and a patient with AD
Scientists have established many models to understand the causes and developments of Alzheimer's disease. Although there are no widely accepted models, currently, there are two models that are quite popular among scientists and both are related to the accumulation of abnormal proteins in the brain. The first hypothesis suggests that the accumulation of amyloid plaques from amyloid-beta protein (Aß) disrupts communication between neurons. Hypothetically, a receptor binds amyloid plaques to protein prions . Prion proteins are protein molecules that do not contain nucleic acid or contain but too short to encode proteins. Prion proteins are readily available in the body and do not cause disease. However, depending on the conditions, prions can change the structure and cause many dangerous diseases, causing degeneration of the nervous system and intellectual impairment such as mad cow disease or Creutzfeldt-Jakob disease on humans. However, the lost function cannot be restored when merely removing amyloid plaques from nerve tissue. Therefore, this hypothesis does not represent the whole problem with the cause of AD.
The second hypothesis relates to tau protein - a protein that helps stabilize microtubules inside the brain's neurons before mechanical and chemical damage. The tau hypothesis for Alzheimer's stresses that tau protein may fall into a state known as the hyperphosphilation , in which the protein has absorbed the maximum amount of phosphorus. At this point, they began to assemble themselves into spiral tangles and straight strands. These plexus affects the structure of neurons as they form, narrowing the function of each neuron and eventually destroying the cells. Another potential difficulty associated with tau proteins is that if they are misleading, they can become insoluble sediments, damaging the ability of neurons to function. This once again shows the link to brain aging diseases that are known.

The complete model of Yale University for the amyloid hypothesis shows the new role of mGluR5 when linking prion proteins and Fyn
In a previous study of the amyloid hypothesis , Professor Stephen Strittmatter's team at Yale University demonstrated that short segments of the protein beta-amyloid bind to prion proteins at the membrane of the neuron neuron sutra. Subsequently, the binding of amyloid and protein prion activates Fyn - a contact protein in cell metabolism. Finally, this activation leads to a decrease in the number of synapses (synapses) and tau proteins that are characteristic of AD.
The Yale team has just published their findings in the medical journal Neuron. They concluded that Fyn's activation occurred during the modulation of a protein within the cell membrane and the metabotropic glutamte receptor 5 (mGluR5) . These receptors and antagonists have been studied in the past to treat patients with Fragile X symptoms - an inherited form of autism.
When these drugs are injected into laboratory mice with brain damage similar to Alzheimer's disease, the ability to remember past, present and future memories of rats was restored. feedback Thereby, the inhibition of the signal pathway of the mGluR5 receptor demonstrated greater efficacy than amyloid plate removal therapy when treating the above symptoms in mice.
Stephen Strittmatter said: "The most interesting thing is that in all the links in the molecular chain, this is probably the most vulnerable cricket protein with antagonists. Here, we hope to be able to find one. drugs that reduce complications of Alzheimer's ".
However, researchers still have a lot of work to do. First, they need to find out if similar treatments in mice have similar efficacy for AD patients. After that, they will have to analyze the safety of the drug for use on elderly patients. In addition, the level of injury to the brain is unclear when using mGluR5 therapy. So it may take many more years for Yale's research to bring joy to patients suffering from Alzheimer's complications.
- Russia successfully assembled the latest artificial heart valve model
- Tesla self drive to take the employer to work, self-find place, parking neatly
- Tesla Model X officially launched electric SUVs
- The emergence of the universe simulation model is fast and unbelievably accurate
- NASA demonstrates a model of CO2 greenhouse gas
- 3D model of the fetus
- The Tesla Model 3 officially launched, with 346km / 1 charge, costing $ 35,000
- Elon Musk: 'Model 3 will have future-like spacecraft'
- NASA revealed the latest design of the Warp Drive spacecraft
- All you need to know about the electric vehicle Tesla Model 3
- New research on the 'ghost' mystery of the cosmic model
- Electric car Tesla Model X first returned to Vietnam
 Green tea cleans teeth better than mouthwash?
Green tea cleans teeth better than mouthwash? Death kiss: This is why you should not let anyone kiss your baby's lips
Death kiss: This is why you should not let anyone kiss your baby's lips What is salmonellosis?
What is salmonellosis? Caution should be exercised when using aloe vera through eating and drinking
Caution should be exercised when using aloe vera through eating and drinking