Stem cell method helps treat Parkinson's disease in rats
For the first time, a group including MIT researchers introduced treatments for the symptoms of Parkinson's disease in rats by creating artificial stem cells.
The work, published online in the Proceedings of the National Academy of Sciences on April 7, may lead to effective treatment for Parkinson's patients, or degenerative diseases. nervous system caused. However, the researchers point out that the barrier to cell restructuring must be removed first.
Last year, US and Japanese researchers announced that they reprogrammed normal human cells - such as skin cells - as stem cells similar to embryos, that could produce virtually like any type of cell in the body. In December 2007, a group of scientists from the Whitehead Biological Drug Research Institute established the method of reprogramming skin cells into iPS multi-cell stem cells [ii] , which can be used to cure Red blood cell disease appears in mice.
In another discovery recently made by members of the Whitehead Laboratory, nerve cells produced by reprogramming cells can successfully integrate into the brains of animals and displace them. reduce symptoms of neurodegenerative diseases, such as Parkinson's disease.
'This is the first demonstration that the reprogrammed cells can integrate with the nervous system or positively impact neurodegenerative diseases,' said Marius Werning, author and current author. is a postdoctoral researcher at Laboratory Rudolf Jaenisch and a member of the Whitehead Institute, and a professor of biology at the Massachusetts Institute of Technology.
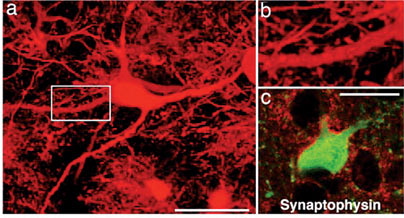
The magnified image taken from the PNAS paper shows that the artificial brain's ability to integrate into the brain is made of stem cells.
In an experiment, Wernig transplanted pre-embryonic neuronal cells in mice, allowing them to live freely and perform analysis after 9 weeks of transplantation. Wernig sees the emergence of new clusters of cells that are born from transplanted cells, which interweave and penetrate brain tissue in the surrounding area. Using the biological research direction guided by Jian-Ping Zhao, the researcher is working at McGovern (MIT) 's Martha Constantine-Paton Laboratory, while analyzing the structure, Wernig also found that pre-neuronal cells penetrate into a few sub-regions of neurons, including neurons and glial cells, and fuse their functions together in the brain.
In another study, Wernig used mice to study samples for Parkinson's disease in humans, caused by the level of dopamine [iii] hormone deficiency in the medial region. Before this mechanism was taken, when dopamine in the brain of rats was removed, the neurons died on one side of the rat brain. In collaboration with Ole Isacson Group of McLean Hospital / Harvard Medical School, Wernig then grafted the dopamine neurotransmitter into the brain region of the mouse called striatum [iv] .
Four weeks after surgery, mice were tested for dopamine-related behaviors. In response to these injections, in typical mouse behavior, they circle in the direction of the brain region with little activity of dopamine. Eight of the nine mice that received the dopamine neuron transplanted had very little activity or even never walked in circles. Eight weeks after transplantation, the researchers found that dopamine neurons had spread to nearby brain regions.
'This experiment shows that in-vitro cell reconstruction can become the fundamental factors that will be used to treat Parkinson's disease,' Jaenisch said. 'It is a challenge for stem cell experiments that are controversial, yes, stem cells can promise the therapies that people often assign to them.'
Jaenisch and Wernig are optimistic that this can be applied to patients, but are also cautious when warning that major challenges have not been eliminated. That means discovering the true causes of cancer or the causes of 'viral feedback' [v] that often convert skin cells into iPS cells, and must find a way. The best solution and the proper location for transplanting neuronal cells into humans.
The study was funded by Ellison Medical Foundation and the National Institutes of Health.
Note:
[i]: Parkinson's: central nervous system degenerative disease due to loss or lack of dopamine or dopamine-producing neurons.
[ii]: induced pluripotent stem cell (iPS: induced pluripotent stem cell). This type of stem cell is made from human skin cells, named after Dr. Shinya Yamanaka (Tokyo University). The work that successfully produced human skin stem cells by Dr. Shinya Yamanaka (Tokyo University) and Dr. James Thomson (Wisconsin University), announced in December 2007, has opened the way. Breakthroughs for the medical industry and disrupting all arguments of ethical barriers to stem cell research.
[iii]: dopamine: is a hormone and neurotransmitter that is common in animals, including both vertebrates and invertebrates. In terms of chemical structure, it is a phenethylamine.
[iv]: striatum (striatum): the brain region produces dopamine neurotransmitters
[v]: The retroviruses, or " retroviruses", are RNA-containing extracellular viruses and perform extracellular biological functions completely independent of the host. They have reverse coding enzymes, intermediate DNA synthesis catalysts to combine with the genes of host cells that they parasitize (reproduced through an intermediate DNA). Because DNA can be created, they can produce proteins that carry genetic information to generations of descendants.
Nam Hy Hoang Phong (translated and annotated by 'Stem cell method treats Parkinson's symptoms in rats' , MIT News)
- China: Many people die from stem cell therapy
- Use blind cured stem cell contact lenses
- Stem cell transplantation to treat 40 critical diseases
- Japanese scientist and stem cell story
- LEARN ABOUT ORIGINAL CELL (Part 5)
- Vietnamese doctors turned umbilical cord into a source of 6 billion stem cells
- The paradise and barrier of human embryonic stem cells
- Mexico focuses on promoting the creation of stem cell banks
- Treatment of deafness by stem cell method
- Application of stem cells in the treatment of chronic obstructive pulmonary disease
- Korea uses stem cells to treat Huntington's disease
- Create human heart from stem cells
 Green tea cleans teeth better than mouthwash?
Green tea cleans teeth better than mouthwash? Death kiss: This is why you should not let anyone kiss your baby's lips
Death kiss: This is why you should not let anyone kiss your baby's lips What is salmonellosis?
What is salmonellosis? Caution should be exercised when using aloe vera through eating and drinking
Caution should be exercised when using aloe vera through eating and drinking